Abstract

Background: Adults with chronic immune thrombocytopenia (ITP) have increased risk of thromboembolism (TE) compared to the general population. Management may be challenging in relapsed/refractory ITP due to risk of bleeding with severe thrombocytopenia. Few studies have examined the management of venous thromboembolism (VTE) in ITP, or outcomes such as recurrent VTE and major bleeding.
Aims: To evaluate the impact of relapsed/refractory ITP on the acute management and outcomes of VTE in adults.
Methods: This multicentre retrospective cohort study included all patients ≥18 years with chronic ITP who received second-line therapy (2012-2020) in the province of Alberta, Canada. Demographics, ITP history and treatment were collected. We also collected major and minor ITP-related thrombotic risk factors including splenectomy status, inflammatory/autoimmune disorders, antiphospholipid antibody syndrome (APS), and use of thrombopoietin receptor agonists (TPO-RA) at the time of VTE. The incidence rate was calculated by dividing the number of VTE events by the person-years of follow-up, from time of ITP diagnosis to time of event, death, or last follow-up. For each VTE event, we examined initial and nadir platelet counts, ITP-directed therapy and quality of anticoagulation. Outcomes included recurrent VTE, major bleeding and deaths from TE and major bleeding. Research ethics approval was obtained.
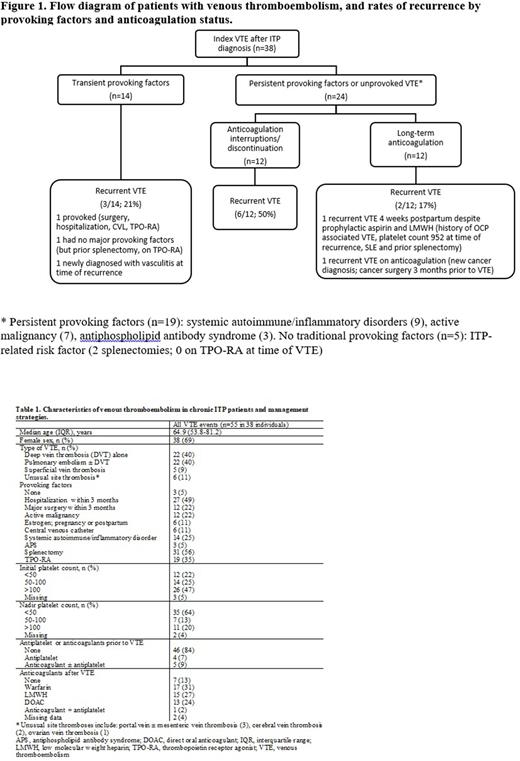
Results: During 2713 person-years of follow-up since ITP diagnosis, 38/326 (12%) developed a total of 55 VTE events. These included: 22 (40%) isolated deep vein thrombosis (DVT), 22 (40%) pulmonary embolism ± DVT, 6 (11%) unusual site thrombosis, and 5 (9%) superficial vein thrombosis (Table 1). The incidence rate of VTE was 1.4 (95% CI 1.0-1.9) per 100 person-years. The median age at the time of VTE was 65 (IQR 54-81) years, 26/38 (68%) were women. Among the 38 index VTE events, half (19; 50%) had a persistent risk factor (active malignancy, systemic autoimmune/inflammatory disorder, APS), 14 (37%) had one or more transient risk factors, and only 5 (13%) were unprovoked VTE (Figure 1). With respect to ITP-related risk factors, 18 (47%) had prior splenectomies, and 7 (18%) received TPO-RA at the time of index VTE.
The median platelet count at the time of VTE diagnosis was 100 x 109/L (interquartile range; IQR 57-260). The median nadir platelet count within 3 months after the VTE diagnosis, however, was only 30 x 109/L (IQR 8-65). Seven (13%) of the 55 VTE events were not treated with anticoagulation upon initial diagnosis due to severe thrombocytopenia (n=4), major bleeding (n=1), or both (n=2). Three patients underwent inferior vena cava filter placement. Another 10 (18%) experienced frequent interruptions or discontinuation of anticoagulation due to thrombocytopenia or major bleeding.
Of the 38 patients, 11 (29%) developed 17 recurrent VTEs at a median of 35.7 months (IQR 2.6-46.6) since index event and 11 (29%) suffered from a major bleed at a median of 21.8 months (IQR 7.9-48.3) since index event (7 intracranial hemorrhages, 4 gastrointestinal bleeding). Among the 24 index VTEs associated with a persistent risk factor or unprovoked VTE, recurrent VTE occurred in 6/12 (50%) individuals who experienced anticoagulation interruptions/discontinuation, compared with 2/12 (17%) individuals maintained on long-term anticoagulation (Figure 1). Of the 14 index VTEs associated with a transient risk factor, 3 (21%) developed recurrent VTE. Twenty-one (55%) died at last follow-up, at a median age of 72 years (IQR 64-83). Common causes of death included: arterial or venous TE (n=5), major bleeding (n=3), infections (n=5), and malignancies (n=5).
Conclusion: Acute VTE is prevalent and potentially life-threatening in a chronic ITP population. Severe thrombocytopenia does not offer protection from VTE development or recurrence, but often renders the optimal anticoagulation choice challenging. With the advances of ITP therapies, aggressive ITP management is critical for optimizing the quality of anticoagulation, while reducing the risk of bleeding and recurrent TE.
Disclosures
Wu:Pfizer, Leo Pharma, Servier, BMS-Pfizer: Honoraria. Sun:Sanofi/Sobi, Shire/Takeda: Honoraria.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal